|
SYMPTOM
|
SINUSITIS
|
ALLERGY
|
COLD
|
Facial Pressure/
Pain
|
Yes
|
Sometimes
|
Sometimes
|
Duration of Illness
|
Over 10-14 days
|
Varies
|
Under 10 days
|
Nasal Discharge
|
Thick, yellow-green
|
Clear, thin, watery
|
Thick, whitish or thin
|
Fever
|
Sometimes
|
No
|
Sometimes
|
Headache
|
Sometimes
|
Sometimes
|
Sometimes
|
Pain in Upper Teeth
|
Sometimes
|
No
|
No
|
Bad Breath
|
Sometimes
|
No
|
No
|
Coughing
|
Sometimes
|
Sometimes
|
Yes
|
Nasal Congestion
|
Yes
|
Sometimes
|
Yes
|
Sneezing
|
No
|
Sometimes
|
Yes
|
Acute Community-Acquired Sinusitis: A Review of Epidemiology and Management
Jeffrey Lauer, MD
Infect Med 20(1):44-48, 2003. © 2003 Cliggott Publishing, Division of SCP Communications
Posted 02/28/2003
Abstract and Introduction
Abstract
Acute sinusitis has multiple viral and bacterial causes and may affect any of the paranasal sinuses. Viral rhinosinusitis is extremely common, and as many as 2% of cases are complicated by acute bacterial sinusitis. Clinical findings have limited sensitivity and specificity, and initial treatment is usually empiric. When complications such as orbital cellulitis occur, sinus CT scans and cultures may be required to guide therapy.
Introduction
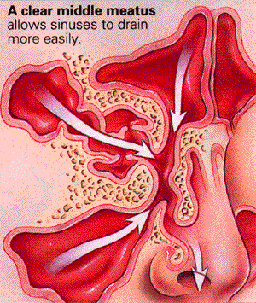
The paranasal sinuses are aerated cavities in the bones of the face that develop as outpouches of the nasal cavity and communicate with this cavity throughout life. The maxillary and ethmoidal sinuses are present at birth; the frontal and sphenoidal sinuses develop after ages 2 and 7 years, respectively.[1] The sinuses reduce overall skull weight, participate in warming and humidification of inspired air, and add resonance to the voice. The sinuses are lined with ciliated pseudostratified epithelium containing mucus-producing goblet cells, similar to the lining of the nasal cavity but with less density.[2] The beating cilia carry mucus and contaminants out of the sinuses toward the sinus openings (ostia) at a speed of up to 1 cm/min.[3] The mucous blanket changes 2 to 3 times each hour.
Obstruction of the ostia and/or delay in mucociliary transport leads to accumulation of secretions and subsequently to the development of sinusitis. Unlike the nasal passages, the paranasal sinuses are normally sterile. The mechanisms maintaining this sterility include the mucociliary clearance system, the immune system, and possible nitric oxide production within the sinus cavity.[4,5]
The classification of sinusitis can be based on a number of factors, including the patient's immune status, the causative pathogen (viral, bacterial, fungal), and the duration of the sinusitis (acute, subacute, chronic, recurrent). Acute sinusitis is defined as sinusitis lasting 4 weeks or less, while sinusitis is considered subacute when symptoms persist for 4 to 12 weeks and chronic when symptoms last longer than 12 weeks. During the first 7 to 10 days of illness, it may be difficult to determine whether the symptoms are caused by a viral or bacterial pathogen and to decide whether antimicrobials are indicated. Appropriate classification of the cause is important so that the correct treatment can be defined and instituted and treatment outcomes can be evaluated. This article will focus on acute community-acquired bacterial sinusitis, highlighting various aspects of the other types of sinusitis only to demonstrate relationships, similarities, and differences.
Viral Rhinosinusitis
The maxillary sinus is the one most commonly involved with any type of sinusitis, followed in frequency by the ethmoidal, frontal, and sphenoidal sinuses. The most common precursor to bacterial sinusitis is a viral infection of the upper respiratory tract, referred to as viral rhinosinusitis (VRS). VRS is defined as an initial viral syndrome resulting in thickening of sinus mucosa, possible obstruction of the ostia, and the signs and symptoms of classic sinusitis with or without rhinitis. It is unclear whether the presence of the virus in the sinus is needed for the sinus symptoms or whether symptoms result solely from the associated inflammatory response. VRS usually resolves within 7 to 10 days without specific therapy. Two new antiviral agents, pleconaril and AG7088, are currently being evaluated as therapies for VRS caused by rhinoviruses or enteroviruses. It is hoped that these will be effective in shortening the clinical course of VRS.
Epidemiology and Causes of Acute Bacterial Sinusitis
It is estimated that 0.5% to 2% of cases of VRS are complicated by clinically evident acute bacterial sinusitis. In the United States, the incidence of VRS is estimated to be 2 or 3 episodes per year in adults and twice that number in children. Using the US population and an average 4 VRS episodes per year, an estimated 1 billion cases of VRS occur annually, with an expected progression to acute bacterial sinusitis in up to 20 million patients.[2] The 1997 data from the National Ambulatory Medical Care Survey indicated 959.2 million ambulatory care visits, of which 2.8 million were for presumed acute bacterial sinusitis.[6] Thus, it would appear that 1 in 100 patients with VRS and 1 in 10 patients with acute sinusitis seek physician care for their illness.
VRS and its complication of acute bacterial sinusitis have seasonal patterns of occurrence based on the virus involved. In early fall and late spring, rhinovirus is the most common cause, while in winter and early spring, the likely agents are coronavirus, respiratory syncytial virus, and influenza virus. Acute community-acquired sinusitis can result from other causes that demonstrate no particular seasonal pattern, such as swimming (with microaspiration of water into the upper airway); allergies; and nasal obstruction secondary to polyps, tumor, or foreign bodies. Also, those persons with defects in immunity (eg, those with HIV infection or agammaglobulinemia), delayed or absent mucociliary activity (eg, those with Kartagener syndrome or cystic fibrosis), structural defects (eg, those with cleft palate), or functional abnormalities of white blood cells (eg, those with chronic granulomatous disease or Wegener granulomatosis) are at risk for acute sinusitis that may occur regularly or progress to chronic sinus disease.
Dental infections may cause 5% to 10% of all cases of maxillary sinusitis; the roots of the upper back teeth (second bicuspid, first and second molars) abut the floor of the maxillary sinus. Also, smoking may be implicated as a causative factor by means of smoking-induced nasopharyngeal lymphoid hyperplasia[7] and reduced ciliary clearance.[8,9]
The pathogenesis of VRS and acute community-acquired bacterial sinusitis is still debated. The most widely investigated viral pathogen is the rhinovirus. It has a unique ability to evade the host defenses in the upper respiratory tract, and in nonimmune volunteers, it has a greater than 90% infection rate after intranasal inoculation.[10] After deposition in the nose, there is presumed transport to the posterior pharynx and attachment to rhinovirus receptor intercellular adhesion molecule 1.[11] It is the resultant inflammatory and parasympathetic responses, rather than any direct cytotoxic effect of the virus, that cause the classic symptoms of the cold and the physical changes noted in the sinuses. Sinus cavity abnormalities were seen on CT scans from 87% of patients with colds; these abnormalities may involve any of the paranasal sinuses (Table 1).
The inflammatory process results in increased mucosal edema, increased mucus production, and delayed or absent mucociliary clearance with eventual ostial obstruction. Without adequate physiologic sinus drainage, bacteria that normally colonize the nasal passages or the pharynx can be deposited into the sinuses when a person sneezes, coughs, or blows his or her nose. This process is believed to account for the development of acute community-acquired bacterial sinusitis following an upper respiratory tract viral illness.
Manifestations of Sinusitis
Symptoms of VRS and acute bacterial sinusitis can include purulent nasal or postnasal drainage, nasal congestion, and sinus pain or pressure. The location of the sinus pain or pressure depends on the sinus involved. Maxillary sinus pain is often perceived as being located in the cheek or upper teeth; ethmoidal si-nus pain, between the eyes or retro-orbital; frontal sinus pain, above the eyebrow; and sphenoidal sinus pain, in the upper half of the face or retro-orbital with radiation to the occiput. Sinus pain is frequently worse when the patient bends forward or is supine. These symptoms, although suggestive of sinus involvement, obviously do not identify the cause. If they occur early in the course of an illness, they may represent a viral or bacterial origin.
The persistence of cold symptoms for more than 7 to 10 days (or longer than usual for a particular patient) is the most consistent clinical feature of acute bacterial sinusitis.[12] Complete opacification of the maxillary or frontal sinus, shown by transillumination with a strong flashlight, constitutes good evidence of sinusitis. However, the differentiation of viral from bacterial sinusitis or a combination of viral-bacterial sinusitis can be difficult.
Many of the clinical findings routinely used to evaluate for sinusitis have limited sensitivity and specificity. The Task Force on Rhinosinusitis of the American Academy of Otolaryngology-Head and Neck Surgery proposed major and minor factors that could be used to tentatively diagnose sinusitis.[13-15] The diagnosis requires the presence of at least 2 major factors or 1 major and 2 minor factors. The major factors include facial pain or pressure, facial congestion or fullness, nasal obstruction, nasal purulence or discolored postnasal drainage, and fever (in acute sinusitis only). The minor factors are headache; fever (in nonacute sinusitis); halitosis; fatigue; dental pain; cough; and ear pain, pressure, or fullness.
Besides the clinical evaluation for sinusitis, radiologic imaging has been used routinely. Four-view sinus x-ray films are helpful when looking for opacity, an air-fluid level, or 4 mm or more of sinus mucosal thickening. CT is more sensitive than routine radiography. In many institutions, the cost of CT limited to the sinuses is comparable to the cost of sinus radiography. Because of their lack of specificity, however, imaging studies are not recommended for the routine diagnosis of community-acquired sinusitis. Patients with VRS have sinus CT scan abnormalities that usually cannot be distinguished from those associated with acute community-acquired bacterial sinusitis,[10] especially early in the disease process.
The viral and bacterial organisms that usually cause acute community-acquired sinusitis have been well identified, especially for the maxillary sinuses (Table 2).[16] The causes have changed little over the years, with maxillary sinus puncture microbiology in 1948 demonstrating Haemophilus influenzae, Diplococcus (Streptococcus) pneumoniae, or Streptococcus hemolyticus (Streptococcus pyogenes).[17] The 3 major bacterial pathogens in acute community-acquired sinus-itis in adults are S pneumoniae, H influenzae (not type b), and Moraxella catarrhalis. In adults, gram-negative bacilli play a role (9% of cases), and anaerobes (6%) are especially important in cases associated with dental infections.
Although clinical symptoms compatible with sinusitis frequently occur in patients with Chlamydia pneumoniae respiratory infections, no studies have demonstrated a causal relationship. In patients with deficits involving humoral and cell-mediated immunity, such as in HIV infection, the involved agents are similar but with an increased incidence of Pseudomonas aeruginosa and Staphylococcus species, as determined from surgical cultures.[18,19]
Treatment
Empiric therapy for acute bacterial sinusitis should be directed against the bacterial pathogens most commonly associated with this infection. Sinus puncture is not indicated in routine cases, and cultures of nasal drainage material are not very reliable.
A number of antimicrobials have broad activity against the usual pathogens associated with acute bacterial sinusitis. The b-lactam antimicrobials that continue to show the best activity against penicillin-sensitive and intermediately resistant strains of pneumococci, b-lactamase- producing H influenzae, and M catarrhalis are amoxicillin/clavulanate, cefpodoxime, and cefuroxime. In communities where there is a high prevalence of penicillin-resistant S pneumoniae (in some areas in the United States, 30% of strains or more are resistant), there is also an associated resistance to many of the other commonly used antibiotics, such as erythromycin, clarithromycin, and trimethoprim-sulfamethoxazole. In this situation, the oral second-generation cephalosporins cefadroxil and cefu-roxime axetil may be effective.
The newer quinolones levofloxacin, gatifloxacin, and lomefloxacin provide excellent activity against both penicillin-sensitive and -resistant S pneumoniae and other sinusitis pathogens.[10] Table 3 lists some drugs used to treat acute community-acquired bacterial sinusitis. A 10-day course of antibiotic therapy for acute bacterial sinusitis is usually effective, but some recommend 14 days. With the initiation of antibiotics for bacterial sinusitis, most symptoms begin to resolve within the first 48 to 72 hours. Failure to improve on completion of appropriate antibiotic therapy should prompt consideration of bacterial resistance, noncompliance, or complicated sinusitis.[12]
Proven ancillary therapy for acute community-acquired sinusitis includes oral decongestants, cough suppressants, NSAIDs, and antihistamines. Expectorants, such as guaifenesin, have theoretical value and are often used but are of unproven value in the treatment of sinusitis.[20 It is best to avoid topical cortico-steroids and decongestants, which, although initially effective, can cause rebound vasodilatation, nasal obstruction, and pharyngeal irritation.
The most common complication of sinusitis is orbital cellulitis. This condition usually arises from the ethmoidal sinuses but may also result from maxillary sinus involvement. Other possible complications include Pott puffy tumor; epidural, subdural, or cerebral abscess; meningitis; and cavernous sinus thrombophlebitis.[1] Patients with complicated sinusitis need CT evaluation to rule out a drainable focus and culture of the sinus to guide intravenous antibiotic therapy. While culture results are pending, treatment with a broad-spectrum parenteral antibiotic, such as nafcillin or ceftriaxone, with or without an aminoglycoside, should be started.
Tables
Table 1. Frequency of sinus abnormalities on CT scan in adults with early common colds
|
 |
||||||
Finding
|
Percentage
|
||||||
Occlusion of Infundibulum
|
77
|
||||||
Abnormality of sinus cavity
|
|||||||
Maxillary
|
87
|
||||||
Ethmoidal
|
65
|
||||||
Sphenoidal
|
39
|
||||||
Frontal
|
32
|
||||||
Adapted from Gwaltney JM Jr. In: Mandell GL et al, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 2000.[16]
|
|||||||
Table 2. Viral and bacterial causes of acute community-acquired maxillary sinusitis
|
 |
||||||
Organism
|
Mean percentage of cases (range)
|
||||||
Adults
|
Children
|
||||||
Viruses
|
|||||||
Rhinovirus
|
15
|
--
|
|||||
Influenza virus
|
5
|
2
|
|||||
Parainfluenza virus
|
3
|
2
|
|||||
Adenovirus
|
--
|
2
|
|||||
Bacteria
|
|||||||
Streptococcus pneumoniae
|
31 (20-35)
|
36
|
|||||
Haemophilus influenzae (unencapsulated)
|
21 (6-26)
|
23
|
|||||
S pneumoniae + H influenzae
|
5 (1-9)
|
--
|
|||||
-Streptococci
|
9 (3-19)
|
--
|
|||||
Moraxella catarrhalis
|
8 (2-10)
|
19
|
|||||
Anaerobic bacteria
|
6 (0-10)
|
--
|
|||||
Staphylococcus aureus
|
4 (0-8)
|
--
|
|||||
Streptococcus pyogenes
|
2 (1-3)
|
2
|
|||||
Gram-negative bacteria
|
9 (0-24)
|
2
|
|||||
Adapted from Gwaltney JM Jr. In: Mandell GL et al, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 2000.[16]
|
|||||||
Table 3. Antimicrobials used to treat acute community- acquired bacterial sinusitis in adults
|
 |
||||||
Drug
|
Dosage
|
||||||
Amoxicillin/clavulanate*
|
875 mg/125 mg q12h
|
||||||
Cefpodoxime
|
200 mg q12h
|
||||||
Cefuroxime axetil*
|
250 mg q12h
|
||||||
Cefadroxil
|
500 mg q12h
|
||||||
Cefprozil
|
500 mg q12h
|
||||||
Levofloxacin*
|
500 mg qd
|
||||||
Azithromycin
|
500 mg on day 1, then 250 mg qd on days 2-5; can repeat at 2 weeks if no improvement
|
||||||
Clarithromycin
|
500 mg tid
|
||||||
*
|
Proved effective by pretreatment and post-treatment sinus aspirate culture.
|
||||||
Adapted from Gwaltney JM Jr. In: Mandell GL et al, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 2000.[16]
|
|||||||
References
Durand M, Joseph M, Baker AN. Infections of the upper respiratory tract. In: Fauci AS, Braunwald E, Isselbacher KJ, eds. Harrison's Principles of Internal Medicine. 14th ed. New York: McGraw Hill; 1998:179-180.
Gwaltney JM Jr. Acute community-acquired sinusitis. Clin Infect Dis. 1996;23:1209-1225.
Ahuja GS, Thompson J. What role for antibiotics in otitis media and sinusitis? Postgrad Med. 1998;104:93-104.
Runer T. Studies of Mucociliary Activity and Blood Flow in the Upper Airways, With Special Reference to Endothelins and Nitric Oxide [doctoral thesis]. Lund, Sweden: Department of Oto-Rhino-Laryngology, Head and Neck Surgery, University of Lund; 1996.
Palm J, Lidman C, Graf P, et al. Nasal nitric oxide is reduced in patients with HIV. Acta Otolaryngol. 2000;120:420-423.
Schappert SM. Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 1997. Vital Health Stat 13. 1999;143:i-iv, 1-39.
Finkelstein Y, Malik Z, Kopolovic J, et al. Characterization of smoking-induced nasopharyngeal lymphoid hyperplasia. Laryngoscope. 1997; 107:1635-1642.
Mahakit P, Pumhirun P. A preliminary study of nasal mucociliary clearance in smokers, sinusitis and allergic rhinitis patients. Asian Pac J Allergy Immunol. 1995;13:119-121.
Brook I, Gordon AE. Resistance to antimicrobials used for therapy of otitis media and sinusitis: effort of previous antimicrobial therapy and smoking. Ann Otol Rhinol Laryngol. 1999; 108:645-647.
Gwaltney JM Jr, Phillips CD, Miller RD, Riker DK. Computed tomographic study of the common cold. N Engl J Med. 1994;330:25-30.
Greve JM, Davis G, Meyer AM, et al. The major human rhinovirus receptor is ICAM-1. Cell. 1989;56:839-847.
Gwaltney JM. Sinusitus. In: Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 4th ed. New York: Churchill Livingstone; 1995: 585-590.
Blumenthal HJ. Headaches and sinus disease. Headache. 2001;41:883-888.
Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Sinus and Allergy Health Partnership. Otolaryngol Head Neck Surg. 2000;123(1 pt 2):5-31.
Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Executive summary. Sinus and Allergy Health Partnership. Head Neck Surg. 2000;123(1 pt 2):1-4.
Gwaltney JM Jr. Sinusitis. In: Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 5th ed. Philadelphia: Churchill Livingstone; 2000:676-686.
Urdal K, Bendal P. The microbial flora in 81 cases of maxillary sinusitis. Acta Otolaryngol (Stockh). 1949;37:20-25.
Rombaux P, Bertrand B, Eloy P. Sinusitis in the immunocompromised host. Acta Otolaryngol Belg. 1997;51:305-313.
Milgrim LM, Rubin JS, Rosenstreich DL, Small CB. Sinusitis in human immunodeficiency virus infection: typical and atypical organisms. J Otolaryngol. 1994;23:450-453.
Wawrose SF, Tami TA, Amoils CP. The role of guaifenesin in the treatment of sinonasal disease in patients infected with the human immunodeficiency virus (HIV). Laryngoscope. 1992;102:1225-1228.
Sidebar: Drugs Mentioned in This Article
|
 |
||||||
AG7088
|
|||||||
Amoxicillin/clavulanate
|
Augmentin
|
||||||
Azithromycin
|
Zithromax
|
||||||
Cefadroxil
|
Duricef, generic
|
||||||
Cefpodoxime
|
Vantin
|
||||||
Cefprozil
|
Cefzil
|
||||||
Ceftriaxone
|
Rocephin
|
||||||
Cefuroxime
|
Kefurox, Zinacef
|
||||||
Cefuroxime axetil
|
Ceftin
|
||||||
Clarithromycin
|
Biaxin
|
||||||
Erythromycin
|
Ery-Tab, generic
|
||||||
Gatifloxacin
|
Tequin
|
||||||
Guaifenesin
|
Multiple products
|
||||||
Levofloxacin
|
Levaquin
|
||||||
Lomefloxacin
|
Maxaquin
|
||||||
Nafcillin
|
Unipen, Nallpen
|
||||||
Pleconaril
|
Picovir
|
||||||
Trimethoprim-sulfamethoxazole
|
Bactrim, Septra, generic
|
||||||
Acknowledgements
The author thanks Dr Michael Sands for his manuscript review and editorial comments.
Jeffrey Lauer, MD, University of Florida and Duval County Health Department, Jacksonville
|
|||||||